Federal Policy Resource
Medicare enrollment revalidation cycle 2: What practice leaders need to know
All Medicare Part A and B providers and group practices are required to resubmit and recertify the accuracy of their enrollment information every five years in a process known as revalidation.
Explore Related Content


Federal Policy Resource
(Dec 2025) HHS Information Blocking and Enforcement: What Medical Groups Should Know Resource

Federal Policy Resource
(Dec 2025) Practice Executive Watch List - Health IT

Federal Policy Resource
(Dec 2025) Understanding the Ambulatory Specialty Model

Federal Policy Resource
(Dec 2025) Work RVU Efficiency Adjustment

Federal Policy Resource
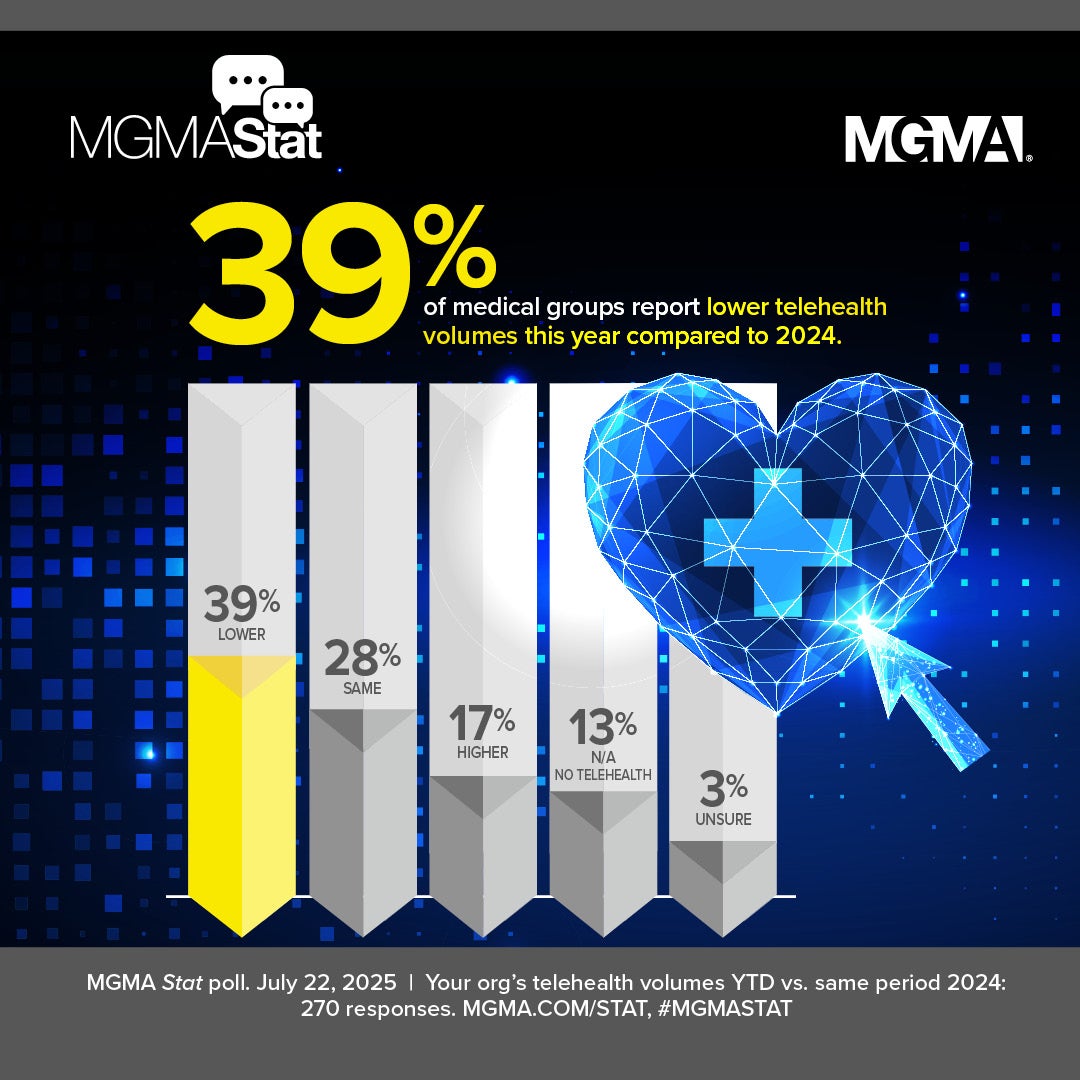
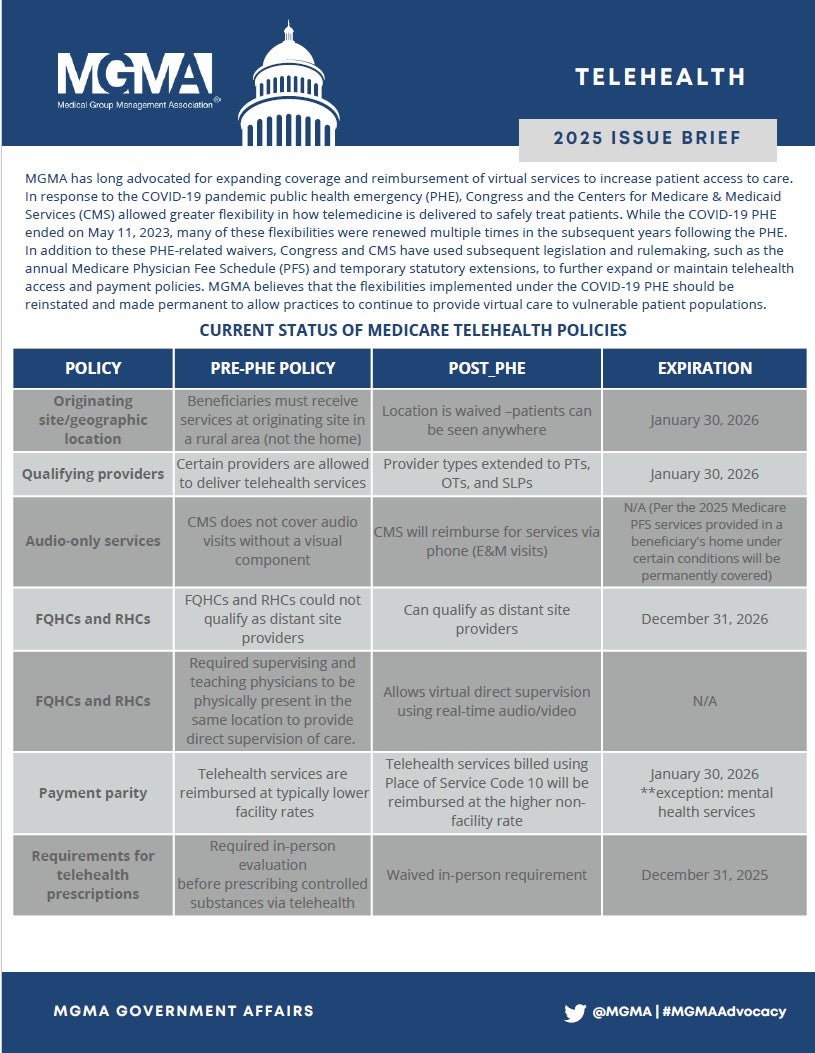
Status of Medicare Telehealth Policy 2025

Federal Policy Resource
Analysis: 2026 Medicare Physician Fee Schedule (PFS) Final Rule for Medical Practices

Sponsored Solution
Value-Based Care and Heart Failure: Evidence on GDMT Adherence
More Federal Policy Resources

Federal Policy Resource
(Dec 2025) Understanding the Ambulatory Specialty Model

Federal Policy Resource
(Dec 2025) Work RVU Efficiency Adjustment

Federal Policy Resource
(Dec 2025) Practice Executive Watch List - Health IT

Federal Policy Resource
(Dec 2025) HHS Information Blocking and Enforcement: What Medical Groups Should Know Resource

Federal Policy Resource
(Dec 9, 2025) Recent Amendments to Medicare Provider Enrollment Regulations

Federal Policy Resource
Status of Medicare Telehealth Policy 2025

Federal Policy Resource
(Nov 2025) Unlocking The ACA Tax Credit Debate

Federal Policy Resource
Analysis: 2026 Medicare Physician Fee Schedule (PFS) Final Rule for Medical Practices

Federal Policy Resource
Update from CMS on the Federal Government Shutdown (October 16, 2025)

Federal Policy Resource
(Sept 2025) Medicaid Reform: Informing Your Decision-Making

Federal Policy Resource
Analysis: 2026 Medicare Physician Fee Schedule (PFS) Proposed Rule

Federal Policy Resource
Increased Immigration Enforcement: Implications for Medical Groups
Federal Policy Resource
Information Blocking Toolkit for Medical Groups

Federal Policy Resource
Analysis: 2025 Medicare Physician Fee Schedule Final Rule

Federal Policy Resource
FTC noncompetes final rule

Federal Policy Resource
Implementing the No Surprises Act
Federal Policy Resource
Analysis: Final 2024 Medicare Physician Payment and Quality Reporting Changes