You're Viewing — Key Insights: 2025 Management and Staff Compensation
Would you like access to the full report? Become an MGMA member today to get full access to this report and much more. (Already a member? Login here.)
Key Insights: 2025 Management and Staff Compensation Data Report
A structural reset is underway for pay benchmarks across management, administrative, and clinical support roles in America’s medical practices, according to the latest benchmarks from the 2025 MGMA DataDive Management and Staff Compensation survey data set, compiled from more than 4,300 medical groups nationwide.
A new report detailing key findings from this year’s data, titled Talent Tug-of-War: Budget Breakers and Opportunity Makers, spotlights a sharp rise in healthcare management and support staff pay, surpassing most increases seen in the past decade. These shifts mark a new reality that practices cannot ignore when planning budgets or hiring strategies.
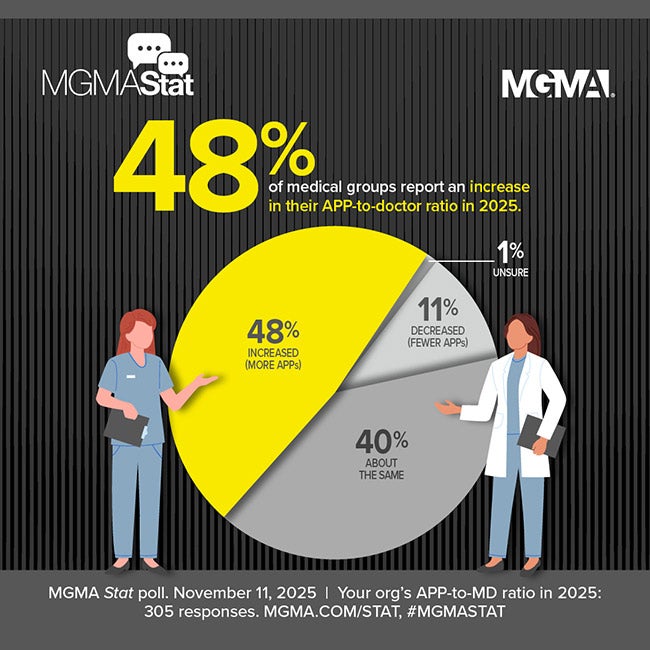
Recruiting is harder, competing offers are inflating salaries, and experienced staff are increasingly hard to replace. The latest upward trend in compensation is not a response to short-term labor disruptions, but rather a reflection of longer-term recalibration of the workforce. In addition to sustained wage pressures, medical groups require new frameworks in planning, budgeting, and retention strategies to navigate regional pay disparities and skillset-specific bidding wars.
Pay Growth Accelerating
Between 2015 and 2024, wages rose significantly across all areas of ambulatory care. The biggest jumps were seen in management and nursing roles:
- Executive Management: +45.6% median compensation growth (2015–2024)
- Senior Management: +38.8%
- General Management: +39.6%
- Supervisors: +36.3%
Administrative support roles also saw major gains: Pay for general accounting staff jumped 52.1% for the decade, and managed care administrative roles rose 39.1% — clear signs that practices are placing more value on staff who handle finances and payer operations.
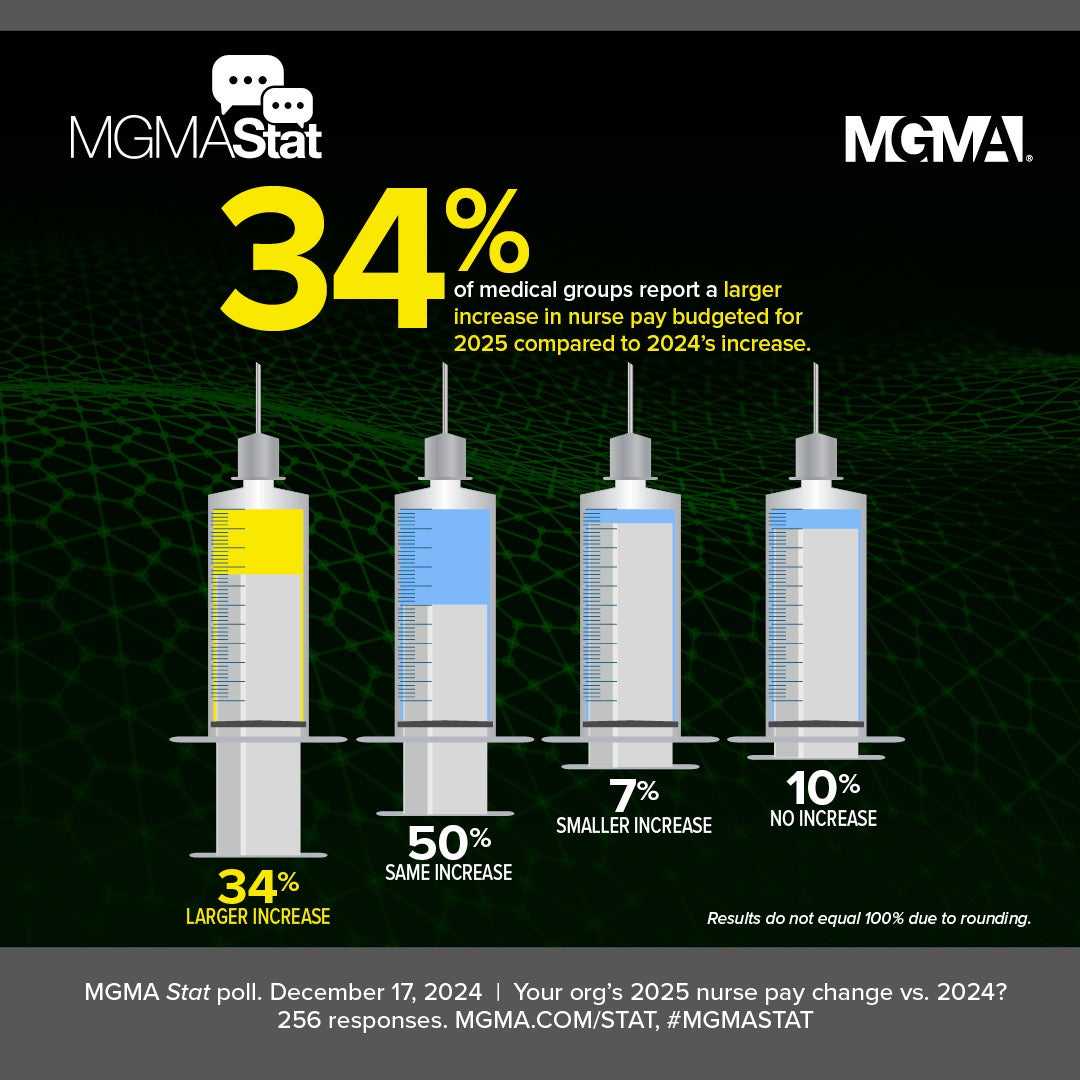
The largest increases were seen in clinical roles:
- Triage Nurses: +84.2% growth in median compensation over 10 years
- Registered Nurses: +64.5%
- Licensed Practical Nurses (LPNs): +49.0%
- Patient Care Assistants (PCAs): Down -0.4% YoY (2023–2024), though still up over five years
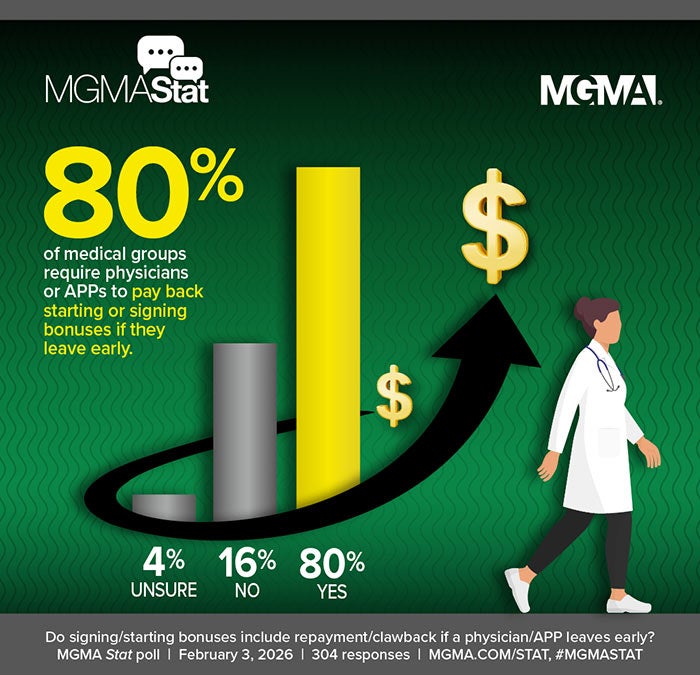
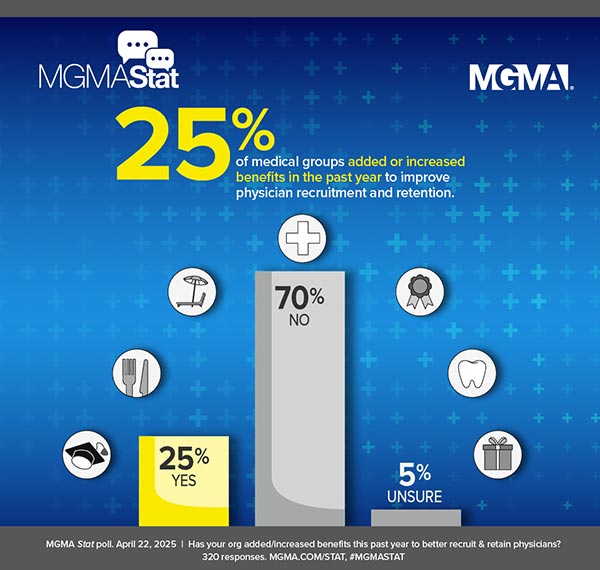
These gains aren’t just about salary — they also reflect growing use of hiring bonuses, retention perks, and richer benefits to hold onto essential staff.
Triage Nurse Compensation (10-Year)
+84.2% (2015–2024)
High demand for digital front door roles and in risk-bearing entities
Registered Nurse Compensation (10-Year)
+64.5% (2015–2024)
ASCs face stiff competition from hospitals, and tele-triage ramping up outpatient demand
Licensed Practical Nurse Compensation (10-Year)
+49.0% (2015-2024)
Growth in home-infusion services and new staffing mandates in SNFs fueling demand
Three Warning Signs for Practice Leaders
What stands out in this year’s findings is not just the size of compensation increases, — it’s the clear signal that legacy compensation models are breaking down:
- Tenure compression: Some long-serving staff now earn less than newer hires doing the same job. This “loyalty pay gap” can lead to morale issues and departures if left unaddressed. Reconciling these imbalances can be a major part of retaining institutional knowledge.
- Diminishing returns on degrees: While advanced degrees still offer a pay bump, that edge is shrinking. The ROI on master’s and doctoral degrees has declined. Many practices may instead prioritize certifications or practical experience — such as payer contract analysis, AI know-how, or expertise in chronic care management — over generalized advanced degrees alone.
- Geographic pay divides: Practices in the Western United States are paying significantly more than those in the South and East, making it harder for some regions to recruit. To stay competitive, lower-paying regions may lean more heavily on remote/hybrid flexibility, signing bonuses, and other incentives to be competitive.

Know exactly what it'll take to attract and keep the right talent. The MGMA Management and Staff Compensation data set analyzes every aspect of a potential hire's characteristics and how it translates to compensation. With its focused insights, you can be confident that your offers and packages will let you attract and retain the talent that fits your practice and your patient needs. You will also get effective, data-driven insights to help you build a healthy nucleus for your organization by empowering everyone and everything surrounding it, including organizational performance.
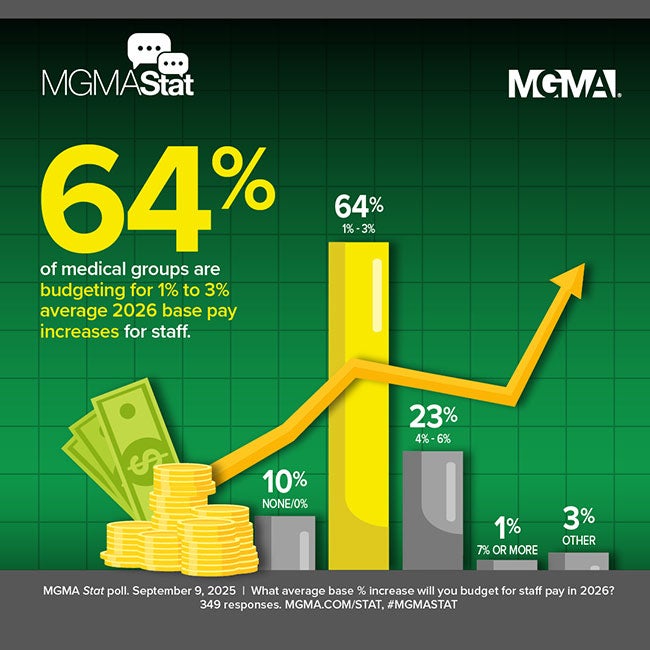
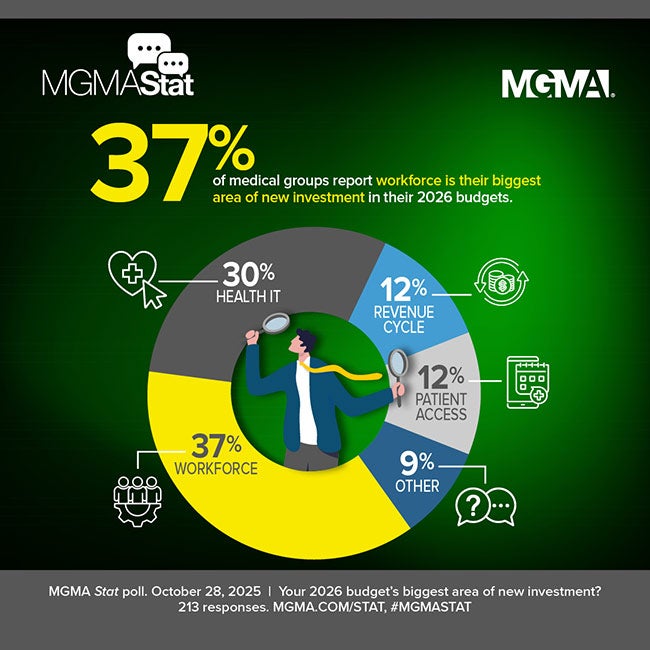
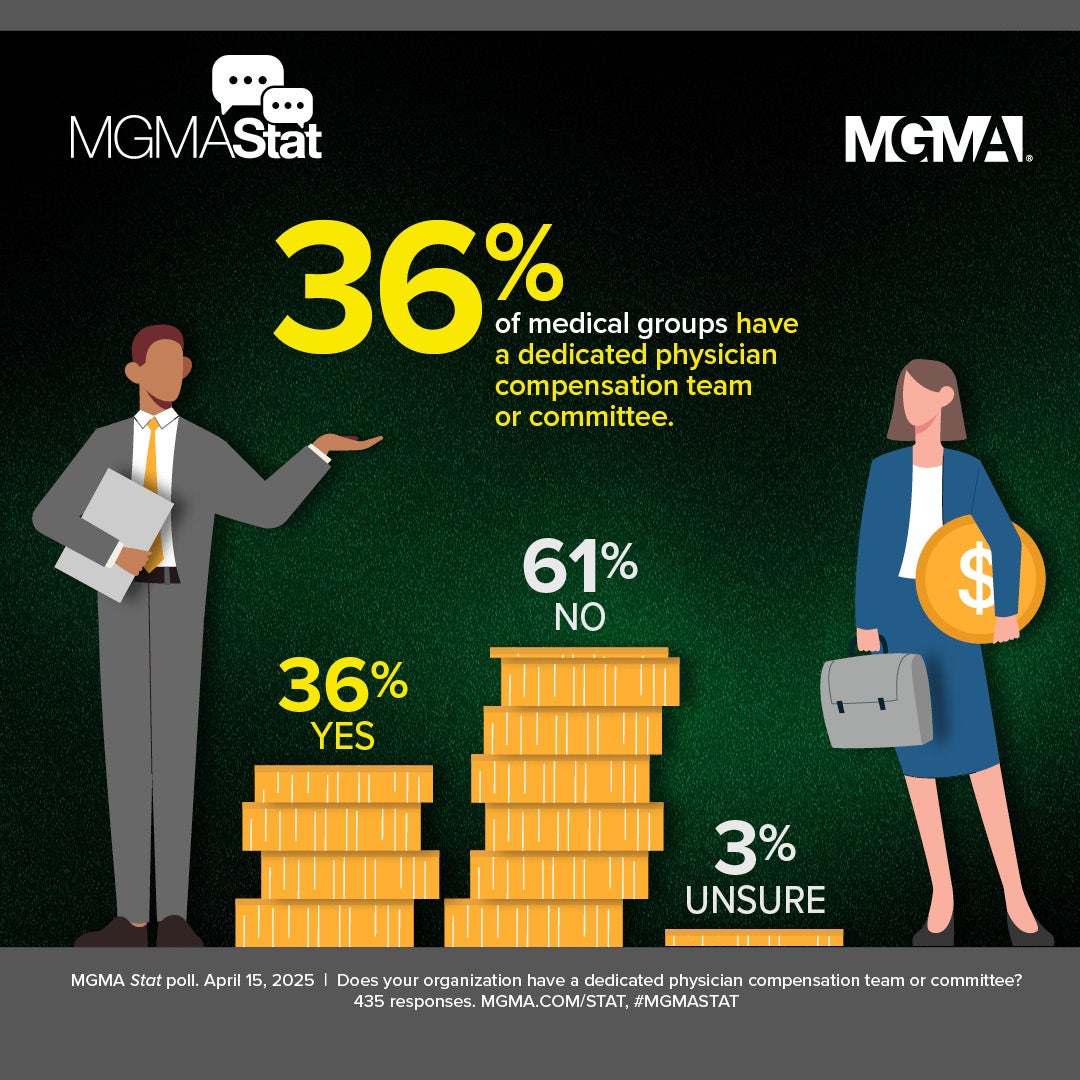
Budget Implications and Compensation Strategy Evolution
For managers and executives planning next year’s budgets, the old rules may no longer apply. Traditional merit increases of 2% to 3% likely won’t keep pace with market trends — shortages of qualified healthcare workers will persist even as other sectors are experiencing a “pink-slip economy” that softens the job market. MGMA’s report outlines several strategies emerging among leading practices:
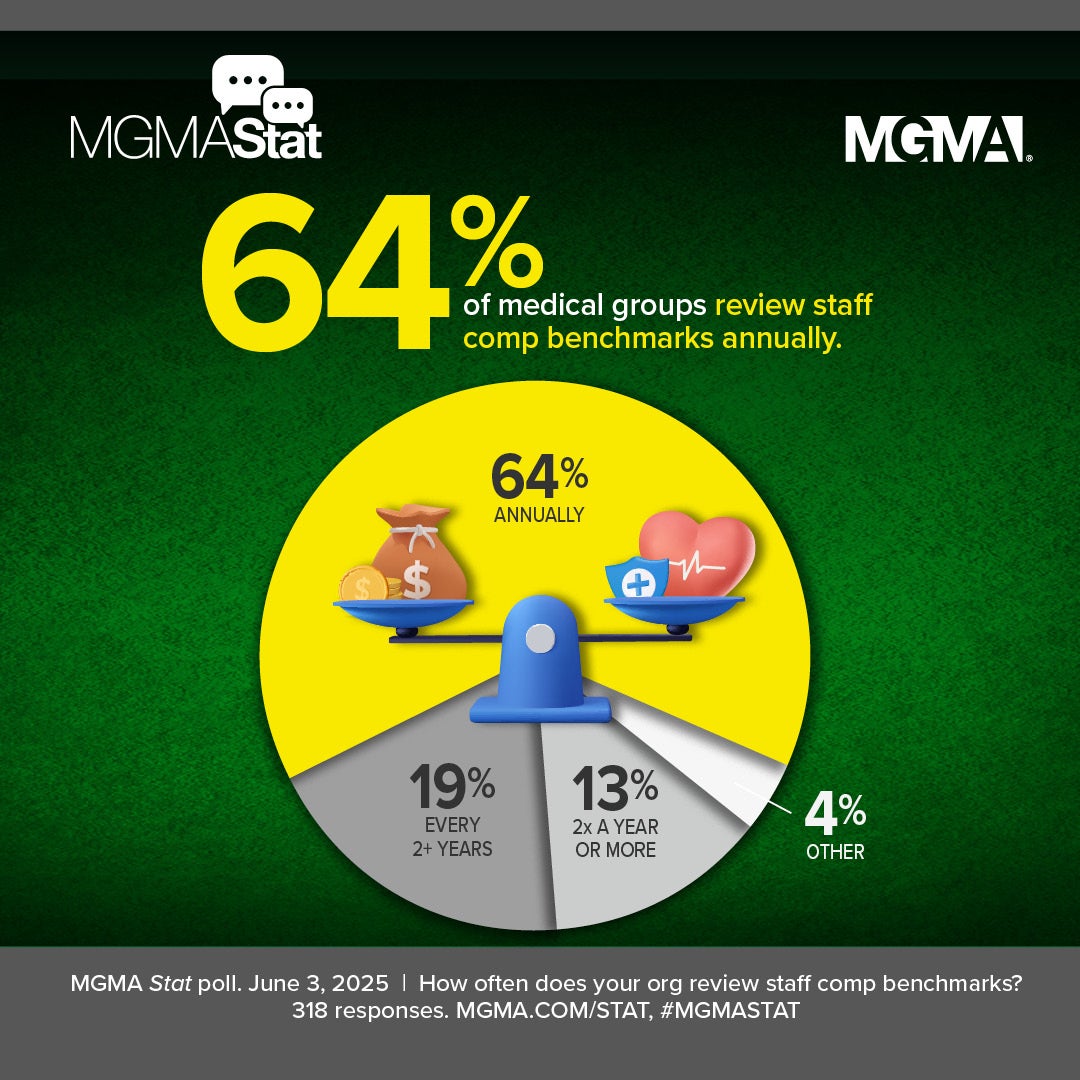
- Re-benchmarking pay bands annually to align with national and regional data
- Investing in strategic skill-building programs for staff taking on more complex roles (e.g., payer contract analysts, data operations, patient access leaders)
- Using flexible pay strategies, such as bonuses tied to billing cycle performance or patient access metrics
- Targeted equity adjustments to address loyalty pay gaps
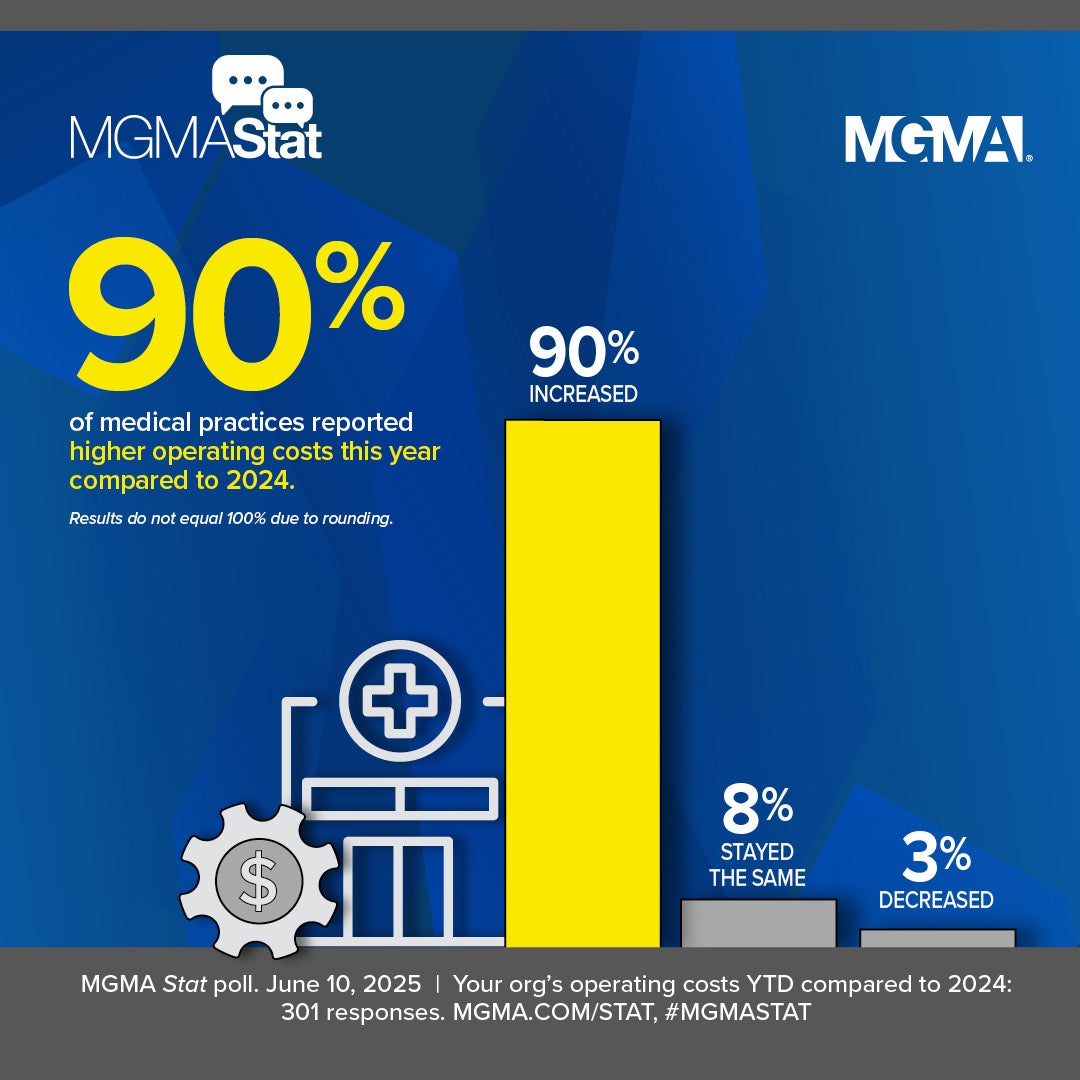
Leaders must also account for cost-of-living increases and growing competition from retail clinics and virtual care providers — both of which influence candidate expectations and turnover risk.
A Defining Moment for Workforce Strategy
The Talent Tug-of-War report arrives at a critical time: Medical groups are facing escalating costs, staffing instability, and evolving care delivery expectations. MGMA’s advice to healthcare leaders? Don’t just chase the market. Build a forward-looking strategy that makes your organization a place where talented staff want to stay.
MGMA Members Get Much More
Get exclusive access to the full report:
- Unmatched depth of pay benchmarks: Access precise year-over-year, 5-year, and 10-year trends for more than a dozen job families, with breakouts by role, region, tenure, and education level.
- Exclusive role-level insights: Discover which roles posted double-digit pay spikes (e.g., triage nurses) and which are seeing pay stagnation or compression.
- Hourly versus total comp analysis: See side-by-side comparisons of how hourly rate increases have (or haven’t) kept pace with total compensation over time.
- Granular regional pay differentials: Examine geographic disparities — e.g., executive managers in the West earn $96K more than their Eastern counterparts, with similarly wide gaps for nurses and support staff.
- Strategic budgeting recommendations: Tap into data-informed guidance on how to forecast labor costs, combat internal pay compression, and prioritize upskilling budgets for 2026.