You're Viewing — Key Insights: 2025 Financials and Operations
Would you like access to the full report? Become an MGMA member today to get full access to this report and much more. (Already a member? Login here.)
Key Insights: 2025 Financials and Operations Data Report
The story of medical practice performance in 2025 isn’t a single metric or a single month. It’s the cascade of minute-to-minute choices that either pull revenue forward or let it slip, that add cost without adding capacity — or unlock time and throughput. This member-exclusive report follows that path from visit to balance, mapping where operating discipline lifts margin and where friction quietly erodes it. You’ll see how small moves — template tuning, same-day salvage, charge-to-post speed, role mix on care teams — roll up to bigger spreads by quarter and year.
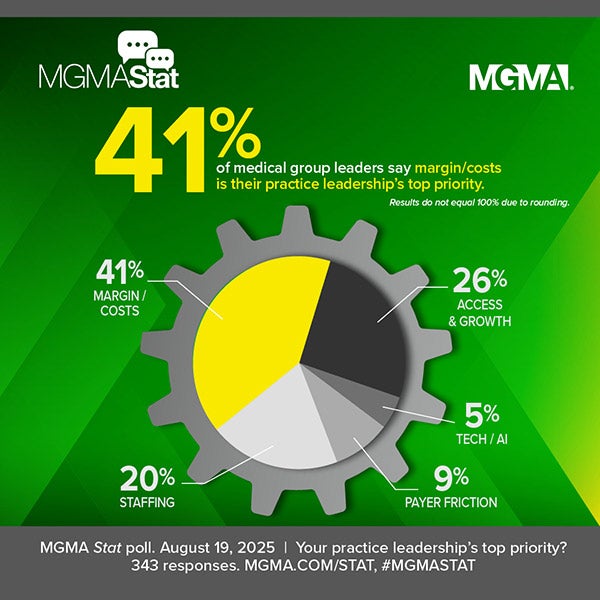
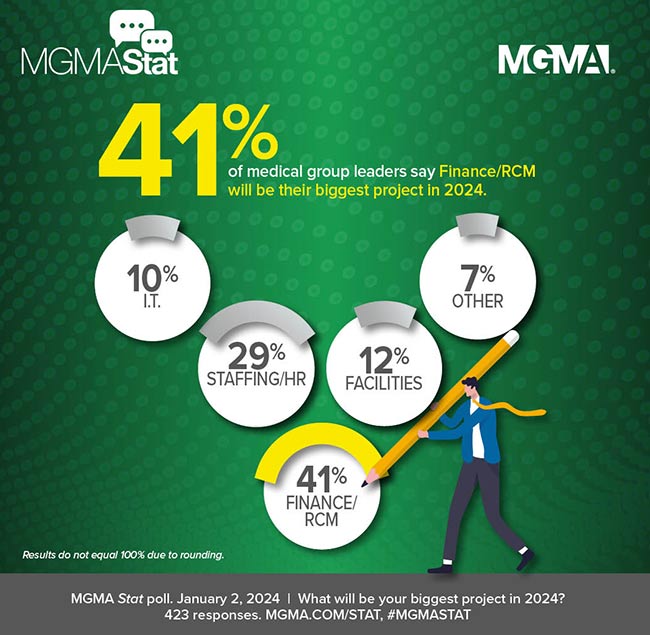
Inside, we track revenue-cost realities by specialty and ownership and translate them into portfolio moves: where to grow, where to protect, and where to rebuild the engine before adding more fuel. We examine the divergence in revenue-cycle health across ownership models and the operational fixes that close cash gaps fast. We also go beyond headcount to “staffing for yield,” using quartiles and role design to show when “more help” truly converts to wRVUs — and when it doesn’t.
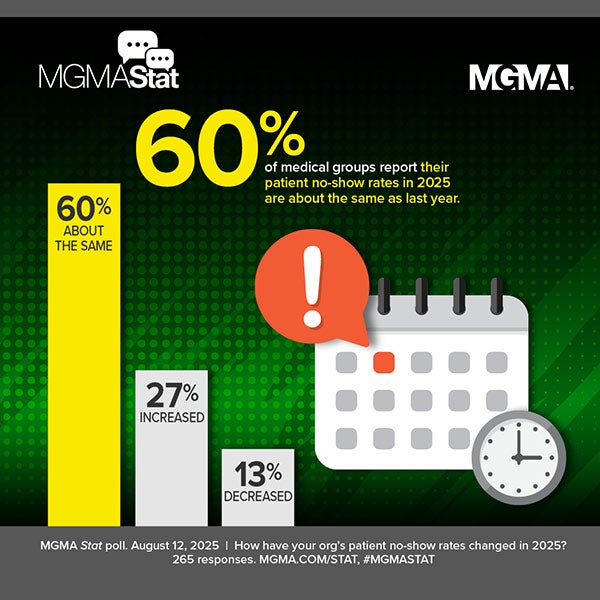
Access is treated as a margin engine, not just a scheduling function. The report quantifies the twin drags of cancellations and slow rebooking, then lays out a salvage funnel — from no-touch rebooking to protected blocks — that captures lost demand while improving point-of-service collections. And because patients increasingly start online, we show where the digital front door is working best (self-schedule and bill pay) and how to connect those pathways to faster cash.
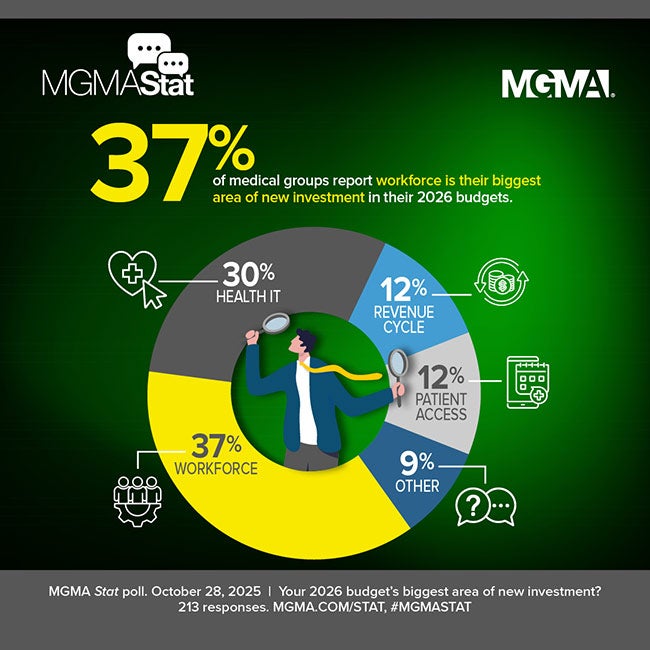
Finally, we package a concise set of KPIs and 90-day plays that leaders are using right now to prepare 2026 budgets: redesigning teams for yield, rationalizing non-labor spend, protecting the top line, and hardening resilience. If you’re deciding where the next dollar of attention, staffing, or technology should go, this is the field guide.
What's inside and how leaders can use it for 2026
- Side-by-side revenue-and-cost trendlines by specialty and ownership to inform portfolio bets (grow, hold, fix).
- “Spread thinking” (revenue minus operating cost) with practical guardrails to size investments and avoid margin drift.
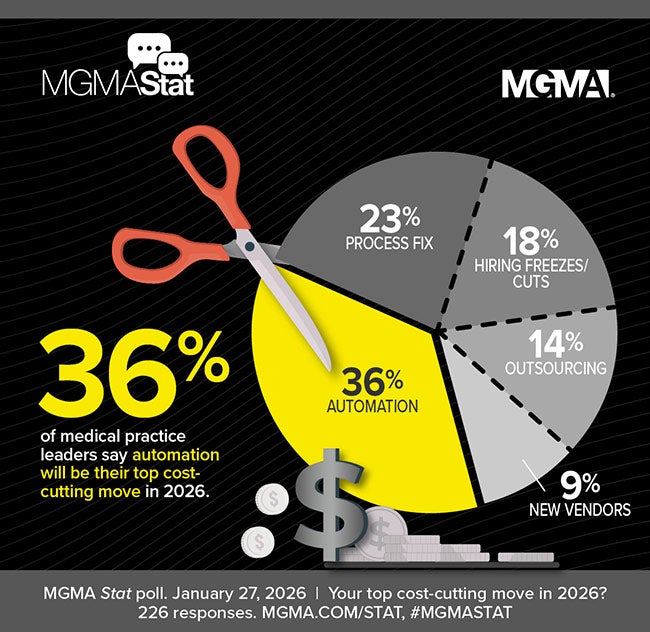
- A clear read on where operating cost pressure is returning and the levers that blunt it without cutting capacity.
- Revenue-cycle health check by ownership (early-cash vs. 120+ exposure) and a fast-track playbook to pull cash forward.
- Billing-ops standards that separate “steady” from “best-in-class” (clean claims, short charge-to-post, targeted denials).
- Staffing-for-yield quartiles: where added support staff correlates with higher productivity—and where workflow must change first.
- APP deployment patterns and role design to expand scope without duplicating physician touch.
- Access friction analysis (cancellations, rebook speed) plus a “salvage funnel” to recapture throughput within 48 hours.
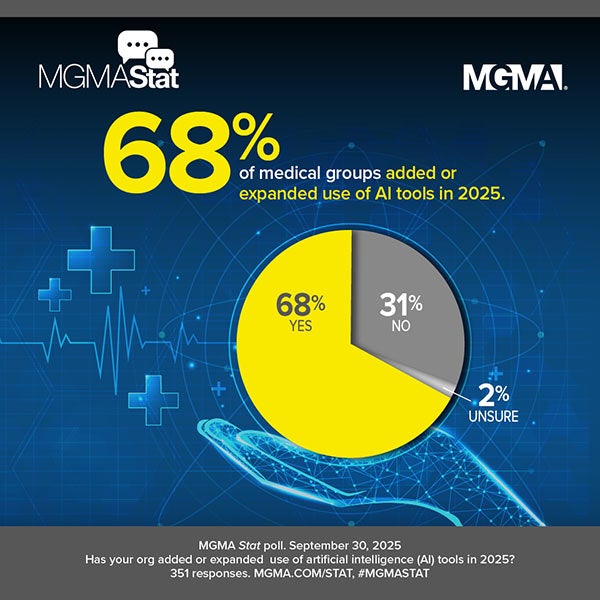
- Digital front door adoption (self-schedule, bill pay) and how to wire it into POS capture and 0–30-day cash.
Want the full data report? Become an MGMA member to access the complete benchmarks and analysis broken down by organization size and guidance for private practices.
$760,383
+3.80% (2023-2024)
Primary Care Total Medical Revenue Per Physician
$697,712
+0.01% (2023–2024)
Nonsurgical Total Medical Revenue Per Physician
$687,652
-2.74% (2023-2024)
Surgical Total Medical Revenue Per Physician

Utilize the Financial and Operations data set to gain precise insight into appropriate head counts to maintain or increase profitability, which might even mean adding, not reducing, staff. Even determine how much you should be spending on staff and other general operating costs and what you should get in return for productivity and profitability. The important insights you gather comparing key performance indicators (KPIs) like hours of operation, wait times, appointment availability, call volume and much more can easily lead to high patient retention and lower employee turnover.
MGMA Members Get Much More
Get exclusive access to the full report:
- Revenue-cost clarity: Track five-year revenue and expense patterns across ownership types and specialties to understand where spreads are widening or compressing.
- Benchmarking beyond averages: See quartile breakouts that reveal where top performers are pulling ahead — and how median practices compare.
- Revenue cycle discipline: Gain insight into charge-to-post times, denial patterns, and A/R aging benchmarks that show where cash is getting stuck.
- Staffing for yield: Examine the relationship between support staff ratios, APP deployment, and physician productivity, with benchmarks to guide role design.
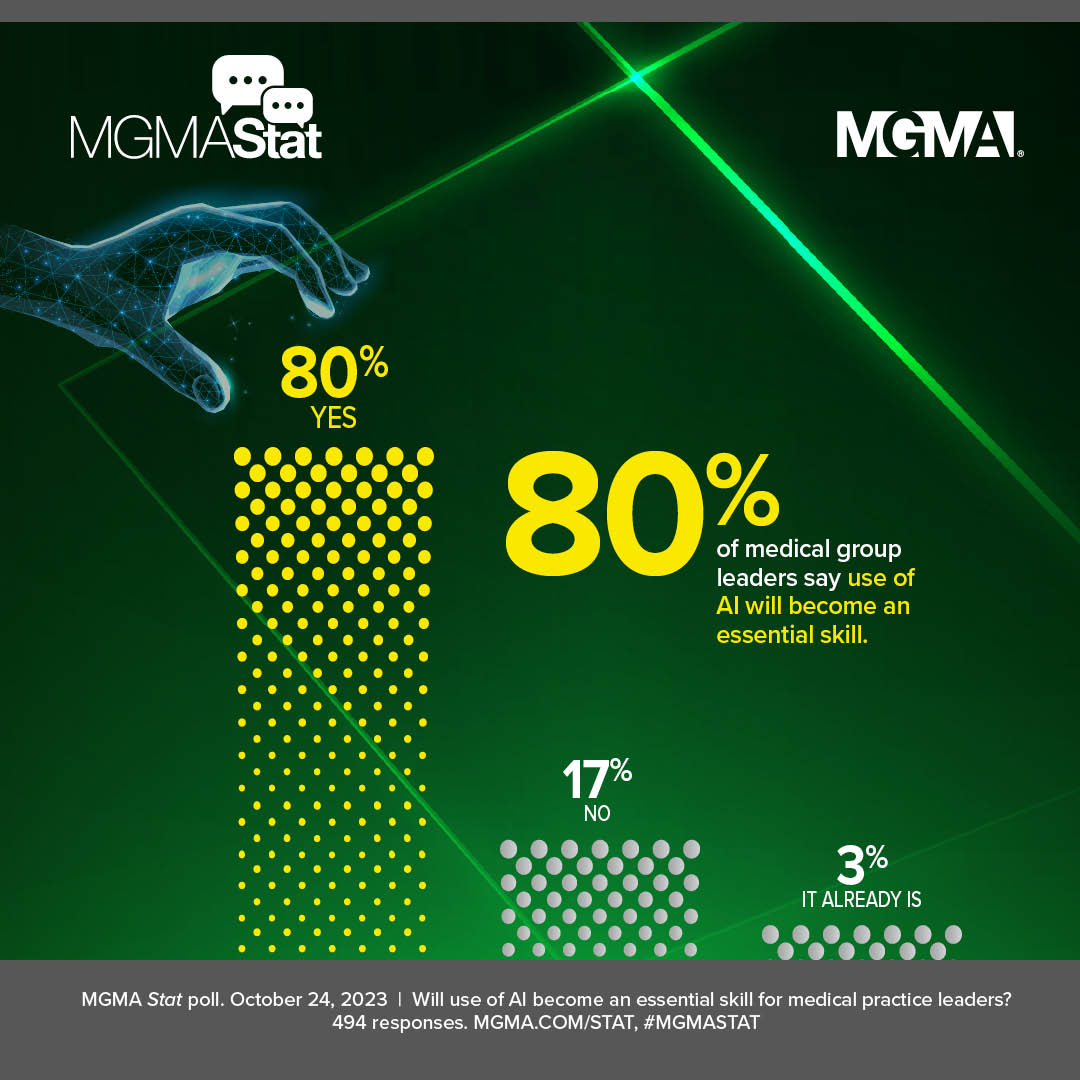
- Digital front door metrics: Understand adoption of online scheduling, bill pay, and patient portals, and their impact on collections and patient engagement.
- Ownership-level insights: Compare operational realities between private, hospital-owned, and health system practices to better position your group for 2026.